In today’s highly regulated pharmaceutical landscape, sampling systems are under the microscope. They’re no longer just mechanical tools, they’re compliance-critical components that can determine whether a facility passes or fails inspection. With the rise of high-potency and sterile manufacturing environments, regulatory agencies like the FDA and EMA have significantly elevated their expectations. As a result, pharmaceutical companies must align their sampling technologies with evolving global GMP standards to avoid costly delays or violations.
This article breaks down how regulatory frameworks influence the design and operation of sampling systems, and how forward-thinking manufacturers are staying ahead of the curve, especially when precision, cleanability, and traceability are on the line.
Why Regulatory Alignment Matters in Sampling
Sampling is one of the most vulnerable steps in the pharmaceutical manufacturing process. It creates a point of contact between the product, the environment, and the operator, opening a window for microbial contamination, mix-ups, or loss of material integrity. That’s why global regulators treat sampling not as an afterthought but as a core compliance checkpoint.
In both FDA and EMA inspections, sampling systems are scrutinized for how well they minimize contamination risks, document traceability, and ensure the sample taken is truly representative. Poorly designed or inadequately documented systems can result in batch rejection, costly investigations, or even facility shutdowns. Regulatory alignment is not just about ticking boxes, it’s about building trust in your processes and products.
How FDA Guidance Shapes Sampling System Expectations
The FDA’s Current Good Manufacturing Practices (cGMP), outlined in 21 CFR Parts 210 and 211, emphasize strict controls at every stage of pharmaceutical production, including sampling. According to §211.84 and §211.160, sampling procedures must ensure that every sample taken is representative, properly identified, and handled under documented procedures. More importantly, the equipment used must be cleanable, calibrated, and designed to prevent cross-contamination.
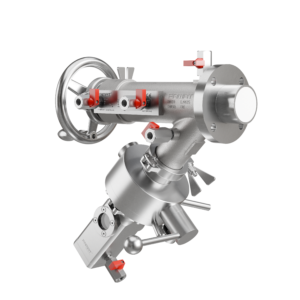
The FDA is particularly vigilant about sampling systems that could compromise product quality through dead zones, difficult-to-clean surfaces, or ambiguous documentation. Modern sampling valves must now provide tool-free disassembly, validated clean-in-place (CIP) or sterilize-in-place (SIP) compatibility, and clear traceability of all materials in contact with the product. If a sampling system can’t demonstrate repeatable, hygienic performance, it’s a liability.
EMA Requirements and the Shift Toward Risk-Based Design
The European Medicines Agency (EMA), through EU GMP guidelines, particularly Annex 1 for sterile products and Annex 15 for qualification and validation, requires that sampling procedures align with a risk-based approach. Instead of mandating fixed rules, EMA expects manufacturers to justify their system choices based on contamination control strategies, cleanroom classifications, and the criticality of the process step.
Under this model, sampling systems are expected to integrate seamlessly into hygienic design principles. This includes flush-to-clean geometry, minimal product hold-up, and full compatibility with aseptic processing or barrier technologies. Additionally, EMA inspectors may request surface roughness specs, cleaning validation results, and documentation of how the sampling system mitigates product and operator risk during both normal operation and failures.
Challenges in Harmonizing FDA and EMA Sampling Requirements
Although the FDA and EMA share the same ultimate goal, ensuring the safety, purity, and quality of pharmaceutical products, their regulatory frameworks differ in subtle but impactful ways. These differences can create complications for global manufacturers trying to standardize equipment and protocols across markets.
For instance, the FDA tends to focus more heavily on consistent documentation and validated procedures, while the EMA emphasizes contamination control within a broader risk-based context. One requires proof of repeatability; the other, proof of justification. For companies exporting globally, this often means:
- Designing sampling systems that meet the stricter requirement of both agencies
- Creating documentation packages that satisfy dual expectations (e.g., US-based traceability standards and EU cleanability data)
- Preparing for inspectors who may prioritize different red flags, even for the same system
Harmonization efforts are underway (e.g., through ICH guidelines), but the reality is that most manufacturers must over-engineer their sampling systems to avoid non-compliance in either jurisdiction.
Impact of Regulatory Focus on Containment and Cross-Contamination
Regulatory agencies are placing increasing emphasis on the ability of sampling systems to prevent contamination, both microbial and cross-contamination between products. The FDA’s focus on aseptic technique, operator exposure, and product sterility means systems must demonstrate not just good design but real-world performance. EMA, meanwhile, prioritizes risk assessments that consider the environment, product type, and exposure scenarios.
For both agencies, this translates into specific scrutiny around dead zones, sealing mechanisms, and whether the sampling path can be completely flushed and sanitized. Systems that are hard to clean, rely on manual disassembly, or introduce air into the process are inherently high-risk. Engineers must design with this in mind, especially in facilities handling multiple non-sterile drug products on shared lines.
Why Material Selection and Surface Finish Matter
Material composition and surface roughness are not just engineering preferences, they’re compliance requirements. FDA inspectors expect full traceability on materials in contact with the product stream, especially for metals and elastomers. This includes documented resistance to cleaning agents, thermal cycling, and degradation over time. EMA regulators place similar importance but often extend it to include chemical compatibility and leachables risk assessments.
Surface finish is also critical. A rough interior surface can trap residue and microorganisms, leading to microbial contamination. Most standards require a surface roughness of Ra ≤ 0.8 µm, but some applications demand electropolishing or passivation. If your documentation doesn’t confirm these specs, you may be forced to repeat testing, or worse, redesign your equipment post-inspection.
Conclusion
In an era of global pharmaceutical manufacturing, the alignment between equipment design and regulatory expectations is not optional, it’s strategic. Both the FDA and EMA now expect sampling systems to demonstrate performance, not just intent. That means validated containment, full material traceability, hygienic design, and seamless integration into cleaning and validation protocols.
Engineers and quality teams that understand these evolving expectations can make smarter choices earlier in the design process. And manufacturers that invest in compliant, future-ready systems, like those leveraging expanding piston or modular technology, will not only pass audits more easily, but gain operational agility in a competitive market.